ACHIEVING PRECISION MEDICATION MANAGEMENT
- Defining Precision Medication Management
- Why Is Precision Medication Management Important?
- What Are the Barriers to Precision Medication Management?
- The Consequences of a Fragmented System
- Why Should Pharmacy Services be Integrated within a Holistic Care Model?
- What Are Interoperability Standards and Why Are They Important?
- How Does the FHIR Standard Address Interoperability Challenges?
- FHIR’s Role in Integrating Pharmacy to Improve Patient Outcomes
- How Do FHIR Standards Enable Innovative Pharmaceutical Programs?
- The Role of Real World Evidence and Real World Data in Precision Medication Management
- How Does a FHIR-Based Platform Support the Use of RWE and RWD?
- Using Smile Digital Health to Enable Precision Medication Management
Author: Nick Zamora
Better Medication Management Series
How a FHIR-based data infrastructure enables the delivery of evidence-based medication management, benefiting healthcare stakeholders and care populations
Precision medication management lies at the intersection of three main pillars of patient care: thorough clinical assessments and planning, accurate prescribing decisions and dynamic patient engagement. When these three categories are optimized and work together, precision medication management can be fully realized. Achieving this ideal state would result in less medication errors, fewer adverse drug events (ADEs), and better outcomes for individuals and healthcare systems.
The following diagram illustrates the three main pillars of patient care and associated medication management programs. When implemented together, they result in a highly optimized model of precision medication management:
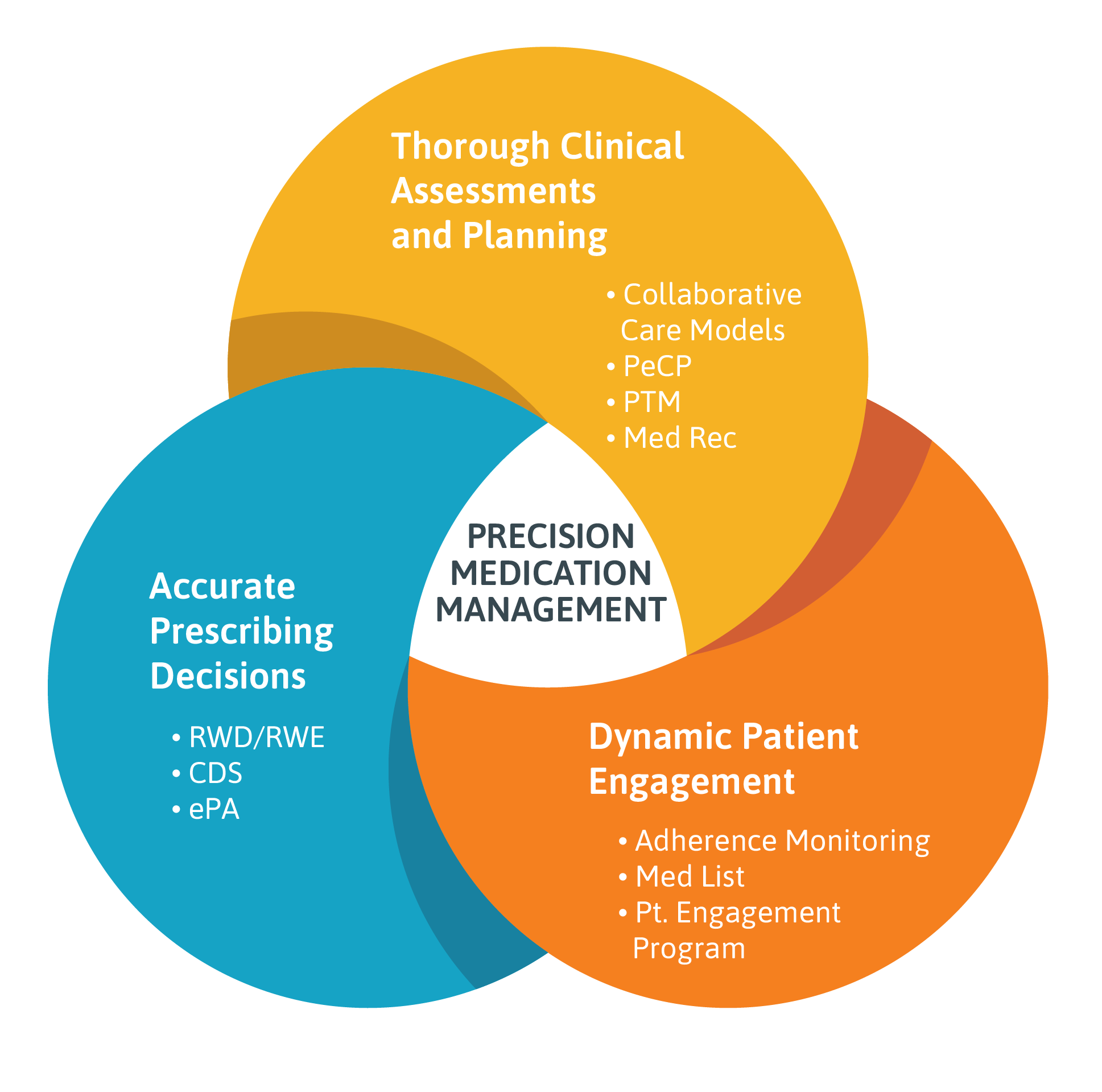
- Thorough clinical assessments and planning are only possible within the framework of a collaborative care model. In this model, providers, pharmacists and other members of a patient’s care team work together and share information. Such a model is enabled by implementation of the Pharmacist eCare Plan (PeCP), an HL7® FHIR® (Fast Healthcare Interoperability Resources) based interoperable platform that provides a common method for exchanging medication-related data.
- Accurate prescribing, in which treatments are optimized for the individual, partly depends on implementing innovative pharmaceutical programs such as Electronic Prior Authorization (ePA) and Clinical Decision Support. Real world data and real world evidence must also be taken into consideration during the prescribing stage and when devising a follow-up plan to ensure patient safety risks are minimized, and outcomes maximized.
- Dynamic patient engagement refers to an approach that emphasizes optimal care delivery, pharmacotherapy management and proactive patient monitoring to ensure adherence to treatment regimens. This patient-centric approach helps ensure individuals are knowledgeable and active participants in their drug regimen, allowing for the proper medication to be taken at the right time, in the correct dose.
Why Is Precision Medication Management Important?
As use of prescription drugs in the US skyrockets, the number of medication errors and ADEs is rising steadily too, with serious—even deadly—consequences. Consider the fact that each year in the US, between 7,000 and 9,000 people die as a result of a medication error. Hundreds of thousands of patients experience ADEs or other medication complications, many of which go unreported.
Beyond the human cost of medication errors and ADEs, there’s also a steep financial toll: The total cost of caring for patients impacted by medication-related errors exceeds $40 billion each year.
With usage of prescription drugs expected to continue to rise in the US, enabling precision medication management is becoming increasingly imperative.
What Are the Barriers to Precision Medication Management?
The overarching hurdle to enabling evidence-based medication management is a fragmented system in which data is siloed and often inaccessible to those who need it most. Breaking this down further, specific barriers can be identified as follows:
1. A Non-Collaborative Care Model That Excludes Pharmacists
Over the years, the role of pharmacists has evolved substantially beyond medication distribution. A pharmacist’s role now includes medication therapy management (MTM), encompassing patient education and therapy optimization by improving adherence and detecting potential ADEs. In fact, in the US, about 65% of Medicare Part D plans now offer MTM delivery through community pharmacists.
While the expansion of their role should be accompanied by greater collaboration between pharmacists and other healthcare providers, in reality, this hasn’t been happening. Pharmacists do not have access to patients’ medication history and there is a lack of communication between them and other members of a patient’s healthcare team. As a consequence, pharmacists often lack the information needed for active medication management.
2. Lack of an Accessible Comprehensive Medication History During Transitions of Care
The absence of a standardized process to obtain and document a complete, accurate list of a patient’s medication history makes proper medication reconciliation impossible. It occurs when healthcare providers work together to ensure accurate medication information is consistently communicated across transitions of care. It requires a systematic and comprehensive review of all medications a patient is taking to ensure that any drugs being added, changed or discontinued are carefully evaluated. Reconciliation enables prescribers to make the most appropriate decisions for patients.
However, there is an absence of a standardized process for comparing a patient’s current medications with medication orders at each point of care transition. As a consequence, about 30% of hospitalized patients have at least one medication discrepancy upon discharge.
3. Unclear Delineation of Responsibilities
In an ideal world, medication reconciliation would be a coordinated effort among healthcare professionals during the transition of care for a patient. However, a lack of clarity around roles and responsibilities for medication reconciliation means no one takes ownership for it. This makes it easy for information to fall through the cracks. Medication reconciliation is also often regarded as an administrative task, which can result in nurses taking over the responsibilities for it, when providers also need to be involved.
The fallout of this situation impacts pharmacists who lack access to a patient’s electronic health records (EHRs). When trying to confirm a patient’s medication information following discharge, pharmacists may have trouble connecting with the hospital doctor, who doesn’t feel responsible for the task of medication reconciliation, or they may be referred to the primary care physician, who may not even be aware that the patient was in the hospital.
The Consequences of a Fragmented System
Achieving optimal patient-centered healthcare in which individuals take the right drugs at the right time and in the right dosage requires a collaborative model of care. This would require all members of the healthcare team to have unfettered access to the patient’s medication history and information, no matter where this data resides. The prevention of medication error and ADEs depends on pharmacists and providers being able to access accurate, up-to-date medication data at the point of care.
Yet the current model does not allow for this: Data is difficult to access, making it impossible to seamlessly transfer important medication information between providers and prescribers, who need this data to guide decision-making. The result is more medication errors, increased ADEs, worse patient outcomes and higher costs to payers and the healthcare system.
Why Should Pharmacy Services be Integrated within a Holistic Care Model?
In an ideal state, patients would receive highly individualized, optimized medication regimens that would in turn optimize their therapeutic outcome. In such a scenario, any potential medication errors would be detected and prevented, as would any potential ADEs. The benefits for individuals and healthcare systems—both from a population health and cost perspective—would be enormous.
Achieving this ideal scenario is not impossible, but its realization depends on fully integrating pharmacy services within a broader vision of delivering comprehensive medication therapy management.
This not only requires rethinking pharmacists’ role within a holistic model of care, but also implementing a data exchange platform that would enable the full integration of pharmacy services within a broader health IT architecture framework.
What Are Interoperability Standards and Why Are They Important?
Enabling a seamless flow of information between clinicians and pharmacists who use different information technology systems depends on the wide-scale adoption of interoperable standards.
Interoperability allows different information technology systems, devices and software applications to communicate, exchange data and use the information that has been exchanged as if it had been generated by the same system. Interoperability among health IT systems is critical to effectively deliver proper care to individuals.
Without interoperability among disparate healthcare IT systems, sharing data in a meaningful way is impossible. Thus a true collaborative care model would not be possible. Interoperability standards create a common vocabulary that enables accurate and reliable communication between different computers and IT systems, providing timely and seamless portability of information with the goal of optimizing the health of individuals.
Interoperability Challenges with EHRs
In the US, over 96% of providers use EHRs as their primary platform for a variety of clinical tasks, including documenting patient information, ordering medications and diagnostic tests and communicating with other providers.
However, EHR technology is at varying levels of interoperability with other health IT systems, including those used by external provider organizations, hospitals and outpatient care facilities. Interestingly, within the same hospital, an EHR may not be operable with the internal pharmacy information system and other internal systems.
A lack of interoperability among different health IT systems—including pharmacy systems—is leading to patient safety events, with the majority being medication-related events.
An evidence-based approach to medication therapy management emphasizes collaboration among healthcare providers to ensure effective and appropriate drug therapy for patients. But this depends upon providers and pharmacists being able to access and share a patient’s medication history, which is only feasible if common interoperability standards are implemented.
Interoperability Challenges in Pharmacy
The pharmacy landscape is divided between community-based and acute care settings which mostly use two separate standards, creating significant data interoperability challenges.
Community pharmacies rely upon the National Council for Prescription Drug Programs (NCPDP), a telecommunications standards development organization, for electronic prescribing, benefit eligibility, billing, dispensing and inventory control. Meanwhile, large healthcare systems and health maintenance groups with acute care pharmacies lean on HL7 standards for data exchange and storage.
Bringing all pharmacy services together to deliver an integrated care model requires translating these two standards so that data can flow seamlessly between both settings. Consolidating claims and prescribing data with health record data presents a challenge as the data resides in siloed systems controlled by busy health IT vendors.
How Does the FHIR Standard Address Interoperability Challenges?
Facilitating a seamless flow of information requires implementation of a data exchange architecture and common standard that allows data to be accessed and shared securely, within all settings and with all relevant stakeholders.
This would address the data interoperability issues identified above, allowing pharmacists access to the information they need to properly complete a comprehensive assessment and share back an optimal medication plan with a patient’s provider team.
Such a model depends on a common standard that facilitates interoperability between systems and devices, allowing clinicians, labs, hospitals, pharmacies and patients to share data no matter which device, application or IT system is being used.
FHIR is the global standard for exchanging healthcare information electronically. Using this standard for an interoperable data exchange platform has many benefits, including:
- Ability to facilitate interoperable exchange with legacy standards
- Ability to transmit only the necessary pieces of information
- Potential for patient-mediated data
A FHIR-based data exchange platform enables precision medication management by ensuring data residing in disparate systems conforms to a common standard. In turn, this ensures information can be easily accessed by clinicians, pharmacists, healthcare facilities and anyone else who needs accurate, up-to-date medication data.
A FHIR-based data platform helps overcome obstacles to precise medication management by:
- Ensuring data never becomes lost or inaccessible, even when patients see multiple providers, are discharged from different hospitals, or use different pharmacies for their prescriptions
- Integrating data from different formats to deliver a comprehensive view of all medications used by a patient
- Linking disparate systems, improving care coordination and optimizing individual care
FHIR’s Role in Integrating Pharmacy to Improve Patient Outcomes
Pharmacy services are increasingly a core component of coordinated care delivery, requiring pharmacists to collaborate not only with one another, but with other members of a patient’s clinical team. This underscores how important ease of access is to patient data and the seamless exchange of medication information between pharmacists in different environments, with other healthcare providers and with patients themselves.
Implementing an interoperable health IT framework based on FHIR standards will help accelerate the advancement of optimal medication management services like MTM and the delivery of point of care medication decision support for programs like chronic disease management and opioid management.
How Do FHIR Standards Enable Innovative Pharmaceutical Programs?
A fully enabled FHIR-based platform addresses the complexities of enabling innovative pharmaceutical programs that enhance the delivery of precision medication management. These programs include:
- Electronic Prior Authorization (ePA)
- Pharmacist eCare Plan (PeCP)
- Clinical Decision Support for Chronic Disease Management and Opioid Management
1. Electronic Prior Authorizations (ePA)
The majority of medication prior authorizations (PA) are still processed manually, which presents several challenges. Manual PA processes are cumbersome. According to the journal Health Affairs, physicians spent more time dealing with drug PAs than any other interaction, absorbing up to eight hours per week. Not only is the PA process time consuming, it leads to delays in patient care. Delayed prescriptions due to PA can lead to patient safety issues. An AMA survey reported that nearly a quarter of providers said a PA-related delay resulted in an adverse health event for a patient, with 16% saying that the delay led to hospitalization.
The solution to this problem is Electronic Prior Authorization (ePA), which speeds up the process by sending PA documents digitally instead of via phone or fax. Integrating ePA into health IT systems can allow providers to easily request PAs. Enabling ePA would allow patients to be provided with their medication in a more timely manner, leading to better health outcomes.
HL7 FHIR is being promoted for ePA of hospital and physician services. However, the FHIR systems needs to work with the payer systems to meet regulatory requirements. These interfaces communicate with an intermediary who can convert the FHIR requests to the corresponding X12 instances prior to passing the requests to the payer. Responses are handled by a reverse mechanism (i.e. payer to intermediary as X12, then converted to FHIR and passed to the EHR in the healthcare facility).
For patients transitioning from an acute care facility to a home setting, the community pharmacy needs to have access to the approved PA before dispensing medication. Making the patient’s record available automatically to the pharmacy, in advance of a patient’s arrival, positively impacts the patient’s experience while reducing the workload for pharmacy staff to acquire this critical information.
2. Pharmacist eCare Plan (PeCP)
The Pharmacist eCare Plan (PeCP) is a FHIR-based interoperable platform that provides a common method for exchanging medication-related information, including care delivery plans, active medication lists, drug therapy problems as well as other data such as lab results and payer information.
The Pharmacist eCare Plan can be used to collect, share and analyze the most important pieces of information, including claims, clinical, laboratory and provider or patient reported data. The PeCP provides an interoperable way to develop a care plan that includes social determinants of health, interventions made by the pharmacy team, clinical goals and referrals to other members of the healthcare team. The aim of the PeCP is to optimize medication use and is dynamic, serving pharmacists who work in different environments.
3. Clinical Decision Support for Chronic Disease Management
Clinical decision support (CDS) provides clinicians, pharmacists, patients and others involved in an individual’s care with person-specific information presented at appropriate times to enhance the delivery of healthcare.
CDS Hooks is a FHIR-based specification that brings authoritative clinical content from outside resources (e.g. blood pressure guidelines from the American Heart Association) into the CDS workflow. CDS Hooks use interoperability standards to connect to the authoritative sources of content. They also have an important role to play in the delivery of precision medication management. When a triggering activity occurs—such as a new medication being prescribed to a patient—the CDS Client notifies each CDS service registered for the activity.
A real world example would be a pharmacist reviewing a patient’s profile prior to dispensing medication. Evidence-based medication prescribing guidelines would be delivered, triggered by the drug description or diagnosis code in the profile. For a patient with Type 2 diabetes, the pharmacist would receive a digital suggestion card with the American Diabetes Association (ADA) medication guidelines. Based on these guidelines, the pharmacist may make a therapy recommendation to the patient’s primary care provider.
Another clinical scenario involves patients who have been prescribed opioid medication for pain management. The prescribing guidelines for opioids are typically in Morphine Milligram Equivalents (MMEs), which is a unit used to calculate a standardized strength of the medication order. Through CDS Hooks, a SMART on FHIR application or a static conversion table could be delivered directly to the pharmacist to ensure the prescription is safe and effective.
The Role of Real World Evidence and Real World Data in Precision Medication Management
As availability of real world data (RWD) and real world evidence (RWE) grows, these sources of information and insight are playing an increasingly greater role in healthcare decisions.
Real world data refers to data relating to an individual’s health status. It can come from a variety of sources, including:
- Electronic Health Records
- Claims and billing data
- Product and disease registries
- Patient-generated data
- Data gathered from other sources that provide health information, such as mobile devices (e.g. wearables)
Real word evidence refers to the evidence regarding the usage and potential benefits or risks of a drug, derived from the analysis of real world data (instead of traditional clinical trials).
When it comes to enablement of precision medication management, real world data provides an alternative source of information that can be used as evidence of a drug’s safety and effectiveness. Where controlled clinical trials are not feasible, real world evidence can help improve patient access to safe, effective medications.
High quality RWE can enhance regulatory bodies’ ability to make informed decisions about the benefits and risks of prescription drugs. For example, the U.S. Food & Drug Administration (FDA) uses RWD and RWE to monitor the postmarket safety of drugs as well as any adverse events, which guides regulatory decision making.
RWD and RWE are also being used to support coverage decisions and the development of support tools for use in clinical practice. Medical product developers are using RWD and RWE to support clinical trial designs and studies to generate new treatment approaches.
How Does a FHIR-Based Platform Support the Use of RWE and RWD?
Leveraging RWD and RWE depends on a data exchange platform that can facilitate the transfer of health information from various sources, allowing data to flow seamlessly among stakeholders in different settings and across different industries.
The collection and transfer of RWD in a standardized way—enabled by an interoperable infrastructure based on the FHIR standard—will become increasingly important as regulatory bodies, payers, pharma companies and other healthcare stakeholders rely more heavily on RWE to inform regulatory guidelines, product development and clinical decisions.
Using Smile Digital Health to Enable Precision Medication Management
Implementing a FHIR-based data exchange platform like Smile benefits patients, providers, payers and pharmacists in different settings by:
- Ensuring all data adheres to a common standard so that it can be easily shared and accessed by providers, pharmacists and members of a patient’s healthcare team, reducing medication errors and ADEs.
- De-siloing medication and health data that resides in proprietary systems, making it accessible to all stakeholders so that it can be used to guide clinical decisions
- Helping clinicians better assess if drugs are bringing value to care populations
- Enabling innovative pharmaceutical programs, such as ePA.
- Helping facilitate access to real world evidence as it becomes increasingly important to regulatory decision making, coverage decisions as well as researchers and pharma companies who use RWD and RWE to support clinical trial designs and observational studies to develop new treatments.
By making data freely available, a FHIR-based clinical data repository such as Smile helps resolve the communication and coordination issues plaguing healthcare systems. By liberating information and helping promote collaboration, a FHIR-based data platform facilitates precision medication management.
How Can Smile Digital Health and HealthChain Inc. Enable Precision Medication Management?
Smile helps institutions and organizations adopt a data-driven, evidence-based approach to clinical care through a data fabric and interoperability platform. By utilizing Smile, digital health company HealthChain has deployed a health information exchange that addresses gaps in drug information and its access, enabling greater precision in the prescribing and use of medications.
